Women are more likely than men to experience chronic pain due to a combination of biological, hormonal, psychological, and sociocultural factors. Hormonal fluctuations, such as those during the menstrual cycle, pregnancy, and menopause, can increase pain sensitivity. Women also have a lower pain threshold and are more prone to conditions like fibromyalgia, migraines, and autoimmune diseases such as rheumatoid arthritis. Additionally, reproductive health issues like endometriosis and psychological factors like stress and anxiety further contribute to higher rates of chronic pain in women. Understanding these factors is key to improving diagnosis, treatment, and management of chronic pain in women.
Common Chronic Pain Conditions in Women
1. Fibromyalgia

Fibromyalgia is a disorder characterized by widespread pain, fatigue, sleep disturbances, and cognitive issues (often referred to as “fibro fog”). Women are diagnosed with fibromyalgia at much higher rates than men. The exact cause is unknown, but researchers believe it involves abnormal pain processing in the brain, often triggered by stress, infections, or physical trauma. The nervous system becomes hypersensitive, amplifying pain signals even in the absence of obvious physical injury.
- Symptoms: Chronic muscle pain, tenderness, fatigue, sleep problems, and difficulty concentrating.
- Treatment: Includes pain relievers, antidepressants, cognitive behavioral therapy (CBT), exercise, and stress management.
2. Endometriosis
Endometriosis is a condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus, often causing severe pain and infertility. This misplaced tissue behaves like normal endometrial tissue—it thickens, breaks down, and bleeds with each menstrual cycle. However, because it has no way to exit the body, it causes inflammation, scarring, and adhesions.
- Symptoms: Severe pelvic pain, painful periods, heavy bleeding, painful intercourse, infertility, and digestive issues.
- Treatment: Hormonal therapies (birth control, GnRH agonists), surgery (laparoscopy), pain management, and lifestyle changes.
3. Migraines

Women are three times more likely than men to experience migraines, largely due to hormonal fluctuations. Estrogen plays a significant role in migraine development, which is why many women experience migraines around their menstrual cycle, pregnancy, or menopause.
- Symptoms: Intense headaches, nausea, sensitivity to light and sound, and sometimes visual disturbances (aura).
- Treatment: Triptans, beta-blockers, CGRP inhibitors, lifestyle modifications, and dietary changes.
4. Chronic Pelvic Pain (CPP)

CPP is a persistent pain in the lower abdominal and pelvic region that lasts for more than six months. It can be caused by gynecological conditions like endometriosis, interstitial cystitis (painful bladder syndrome), or pelvic floor dysfunction. Sometimes, the cause is unknown.
- Symptoms: Dull or sharp pelvic pain, pain during intercourse, urinary urgency, and bowel discomfort.
- Treatment: Physical therapy, pain medications, hormonal therapy, and nerve blocks.
5. Rheumatoid Arthritis (RA)

RA is an autoimmune disease where the immune system attacks the joints, leading to chronic inflammation and pain. Women are affected at three times the rate of men. Hormonal changes (such as pregnancy and menopause) influence the severity of RA symptoms.
- Symptoms: Joint pain, swelling, stiffness, fatigue, and deformities in advanced stages.
- Treatment: Disease-modifying antirheumatic drugs (DMARDs), biologics, steroids, physical therapy, and dietary changes.
6. Osteoarthritis (OA)
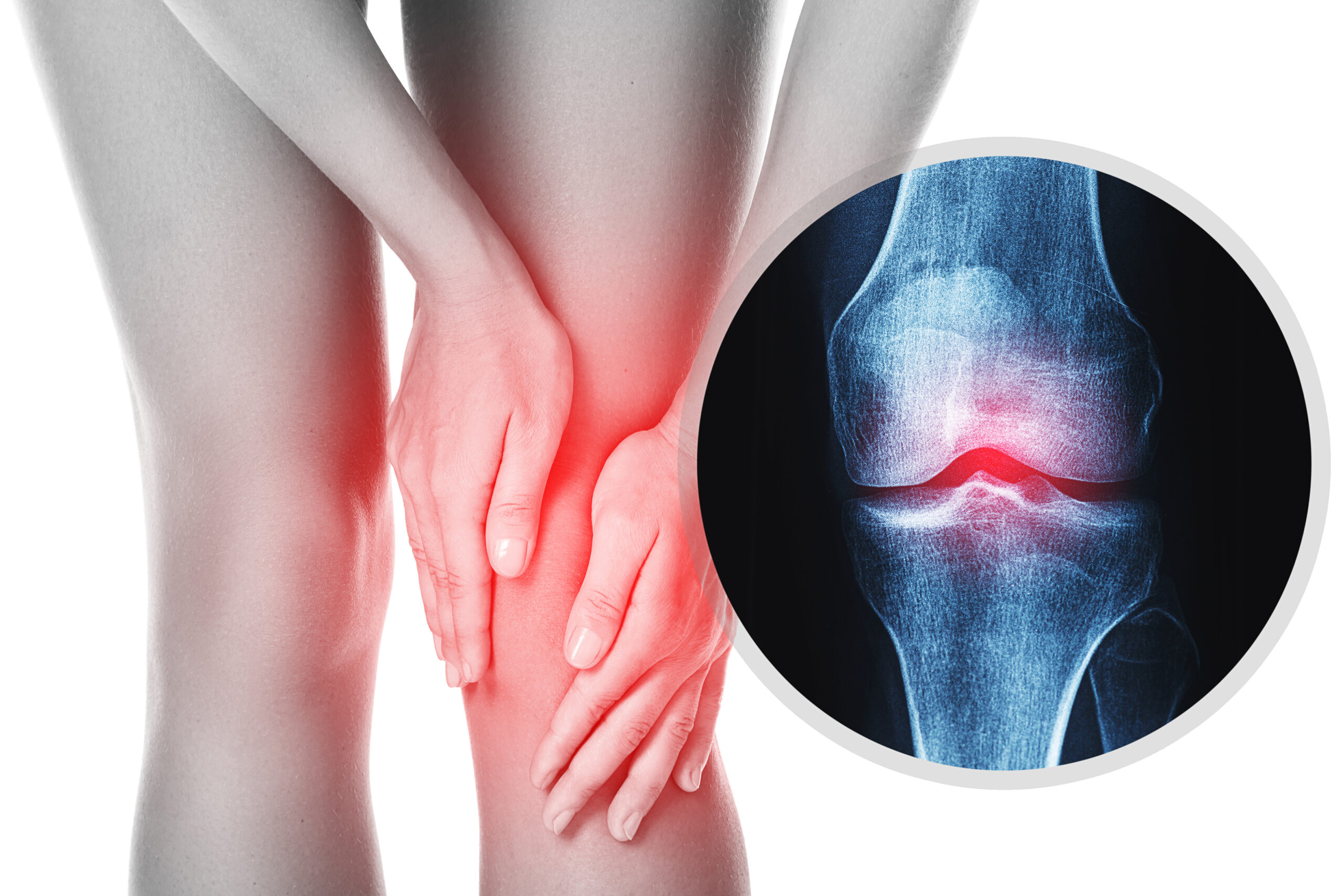
OA occurs when cartilage in the joints wears down over time, causing bones to rub against each other, leading to pain and stiffness. Women have a higher risk of developing OA, particularly after menopause, likely due to hormonal changes that affect joint health.
- Symptoms: Joint pain, stiffness (especially in the morning), swelling, and reduced flexibility.
- Treatment: Pain relievers, physical therapy, weight management, and joint replacement surgery in severe cases.
7. Irritable Bowel Syndrome (IBS)

IBS is a gastrointestinal disorder that causes abdominal pain, bloating, diarrhea, and constipation. Women are more likely to have IBS, and symptoms often worsen during menstruation due to hormonal influences on the gut.
- Symptoms: Abdominal cramps, bloating, alternating constipation and diarrhea, and excessive gas.
- Treatment: Dietary changes (low FODMAP diet), probiotics, medications, and stress management.
8. Temporomandibular Joint Disorder (TMJ)
TMJ affects the jaw joint and surrounding muscles, leading to chronic facial pain, headaches, and difficulty chewing. Women are more likely to develop TMJ due to differences in jaw anatomy, hormonal influences, and higher rates of stress-related clenching and grinding.
- Symptoms: Jaw pain, clicking sounds, headaches, ear pain, and difficulty opening the mouth.
- Treatment: Physical therapy, bite guards, stress reduction techniques, and in severe cases, surgery.
Why Women Are More Affected by Chronic Pain
1. Hormonal Influence
- Estrogen and progesterone influence pain perception.
- Pain sensitivity fluctuates throughout the menstrual cycle.
- Conditions like endometriosis and migraines worsen with hormonal changes.
2. Autoimmune Susceptibility
- Women are more prone to autoimmune diseases like RA and lupus.
- The immune system is more reactive in women, increasing the risk of inflammation-related pain.
3. Nervous System Differences
- Women have a more sensitive pain-processing system due to differences in brain structure.
- Female brains show greater activation in pain-related areas, making pain more intense.
4. Medical Bias and Under-Treatment
- Women’s pain is often dismissed as psychological or exaggerated.
- Studies show that doctors are more likely to prescribe sedatives than pain relievers to women.
- Many chronic pain conditions that primarily affect women (like fibromyalgia and endometriosis) have historically been understudied.
Challenges in Diagnosis & Treatment
1. Delayed Diagnoses
- Many conditions, such as endometriosis and fibromyalgia, take years to diagnose.
- Symptoms are often misattributed to stress, anxiety, or menstruation.
2. Under-Treatment of Pain
- Women are less likely to receive strong pain medications compared to men.
- They are more likely to be told their pain is “all in their head.”
3. Mental Health Stigma
- Women experiencing chronic pain are often labeled as anxious or depressed.
- Psychological factors are considered before medical explanations, leading to misdiagnosis.
4. Lack of Research
- Historically, medical research has been male-focused.
- Women’s unique physiology and pain experiences are still not well understood.
Management & Treatment Options
1. Medications
- NSAIDs (ibuprofen, naproxen) for inflammation.
- Opioids (used cautiously due to addiction risk).
- Neuropathic pain medications (like gabapentin).
- Hormonal treatments for conditions like endometriosis.
2. Physical Therapy
- Helps improve mobility and strengthen muscles.
- Useful for conditions like TMJ, pelvic pain, and arthritis.
3. Lifestyle Adjustments
- Anti-inflammatory diets (rich in omega-3s, low in processed foods).
- Regular low-impact exercise like yoga or swimming.
- Stress management techniques like meditation and deep breathing.
4. Alternative Therapies
- Acupuncture and chiropractic care for pain relief.
- CBD and medical marijuana for pain management.
- Cognitive Behavioral Therapy (CBT) to cope with chronic pain.
5. Support Networks
- Chronic pain support groups (both online and in-person).
- Advocacy organizations that push for better medical research and awareness.
Also read about: The Impact of Social Media on Women’s Mental Health.
conclusion.
women are more prone to chronic pain due to a mix of biological factors, such as hormonal fluctuations and a higher risk of autoimmune diseases, along with differences in how pain is processed in the body. Social and psychological factors, including higher stress levels and caregiving responsibilities, also play a role. Unfortunately, gender biases in healthcare can lead to underdiagnosis and delayed treatment. Greater awareness and research are needed to better understand and address chronic pain in women.
[Link to a related article “Why women suffer more from pain”]