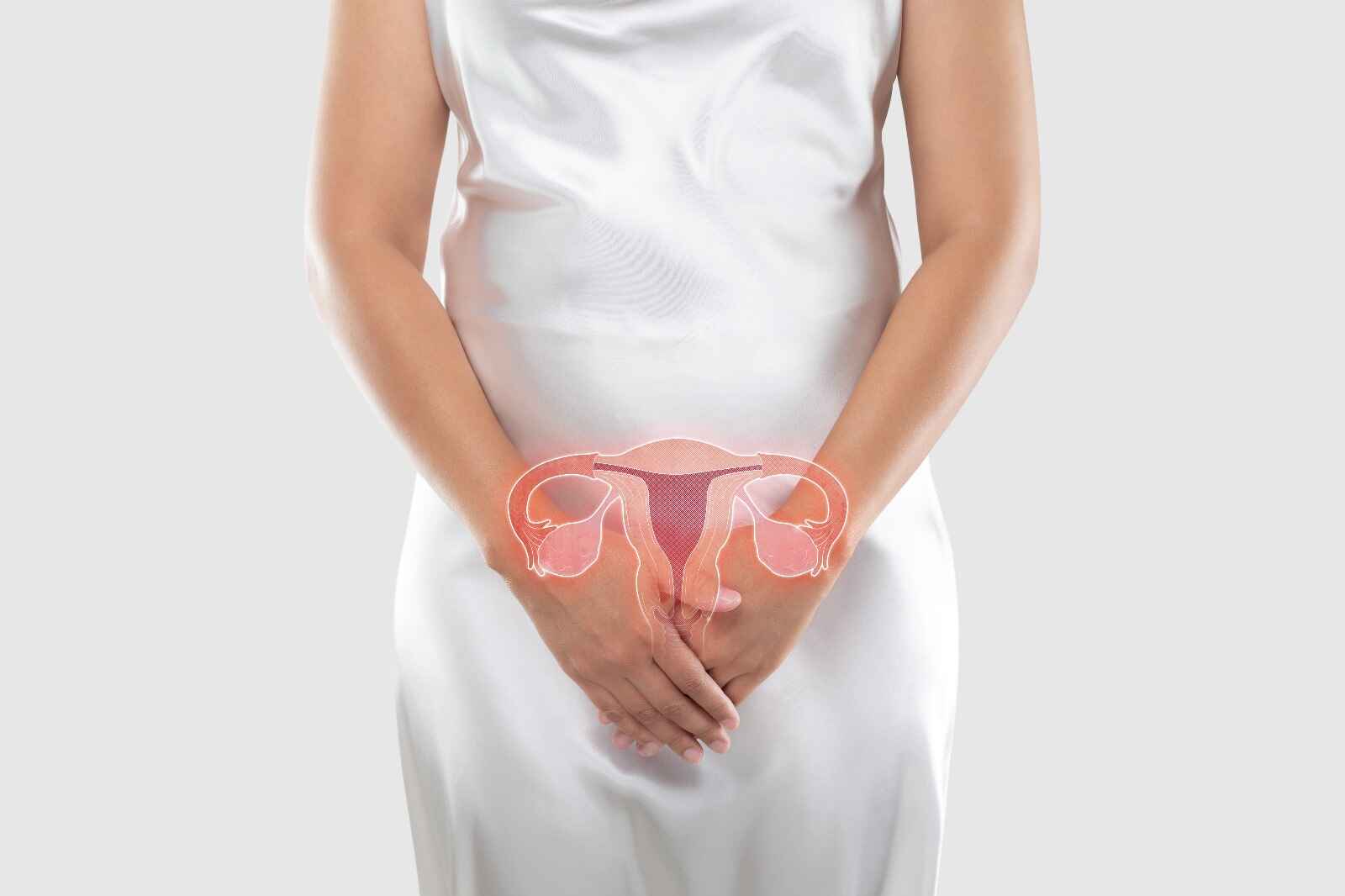
Cervical cancer is a type of cancer that develops in the cervix, the lower part of the uterus that connects to the vagina. It is primarily caused by persistent infection with high-risk human papillomavirus (HPV). The disease can often be prevented through regular screening (Pap smear and HPV test) and the HPV vaccine. Early detection increases the chances of successful treatment.
Early Signs of Cervical Cancer
In the early stages, cervical cancer may not cause noticeable symptoms. However, as it progresses, some common signs include:
-
Abnormal Vaginal Bleeding.
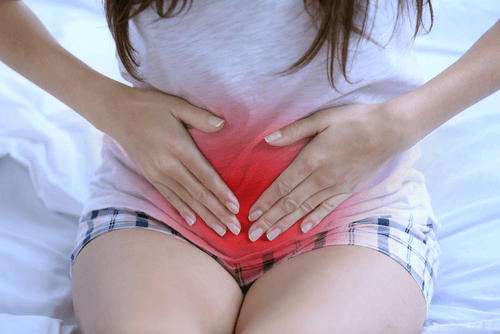
Bleeding between periods, after intercourse, or after menopause.
-
Unusual Vaginal Discharge.
Watery, bloody, or foul-smelling discharge.
-
Pelvic Pain.
 Persistent pain in the pelvic region or pain during intercourse.
Persistent pain in the pelvic region or pain during intercourse. -
Pain During Intercourse.
-
Increased Urination or Discomfort While Urinating.

Pain or frequent urination due to pressure on the bladder.
Cervical Cancer Screening Tests
Regular cervical cancer screenings are crucial for early detection, which can prevent the progression of precancerous changes. The main screening tests for cervical cancer are:
1. Pap Smear (Pap Test).

- What it does: The Pap smear checks for abnormal cell changes in the cervix that could lead to cancer.
- How it’s done: A healthcare provider collects cells from the cervix using a small brush or spatula.
- When to get it: Women aged 21–65 should have a Pap smear every 3 years.
- Why it’s important: Detecting abnormal cells early can lead to treatment before cancer develops.
2. HPV Test

- What it does: The HPV test detects high-risk human papillomavirus (HPV) strains, which are responsible for the majority of cervical cancers.
- How it’s done: A sample of cervical cells is collected, similar to a Pap smear, and tested for HPV DNA.
- When to get it: The HPV test is recommended for women aged 30 and older, typically in combination with the Pap smear.
- Why it’s important: Since HPV is the leading cause of cervical cancer, identifying the virus early can help prevent it.
3. Co-Testing (Pap and HPV Test Together)

- What it does: Co-testing involves both a Pap smear and an HPV test to check for both abnormal cells and high-risk HPV infection.
- How it’s done: Both tests are done simultaneously to provide more comprehensive screening.
- When to get it: Recommended for women aged 30 and older.
Frequency of Screening.
- Ages 21-29: Pap smear every 3 years.
- Ages 30-65: Either Pap smear every 3 years, HPV test every 5 years, or co-testing every 5 years.
- Ages 65 and older: If you’ve had regular screenings with normal results, your doctor may recommend stopping.
Causes of Cervical Cancer.
Cervical cancer is primarily caused by a persistent infection with high-risk strains of human papillomavirus (HPV), a common sexually transmitted virus. Most people who are infected with HPV do not develop cervical cancer, but certain high-risk strains (such as HPV types 16 and 18) can lead to abnormal cell changes in the cervix, which may eventually become cancerous if untreated. Other factors may contribute to the development of cervical cancer, including:
- Weakened immune system (e.g., due to HIV or immunosuppressive drugs)
- Smoking, which damages the cervical cells and increases the risk of cancer
- Long-term use of birth control pills, which has been linked to a slight increase in risk
- Multiple sexual partners, which increases the likelihood of exposure to high-risk HPV strains
Risk Factors for Cervical Cancer.
Several factors can increase the likelihood of developing cervical cancer:
-
HPV Infection
- The most significant risk factor, especially infection with high-risk HPV types.
-
Early sexual activity
- Starting sexual activity at a young age increases the chances of contracting HPV.
-
Multiple sexual partners
- More sexual partners increase the risk of HPV exposure.
-
Smoking
- Smoking weakens the immune system and makes it harder for the body to clear HPV infections.
-
Weakened immune system
- Conditions like HIV/AIDS or immune-suppressing treatments can increase the risk of cervical cancer.
-
Chronic use of oral contraceptives
- Long-term use (over five years) has been linked to a higher risk of cervical cancer, though the risk decreases after stopping the pills.
-
Having many children
- Giving birth to multiple children may slightly increase the risk due to changes in cervical cells during pregnancy.
Treatment Options for Cervical Cancer.
Treatment for cervical cancer depends on its stage, location, and overall health of the patient. Common treatment options include:
-
Surgery.
- Cone biopsy: Removal of a cone-shaped portion of the cervix containing abnormal cells.
- Hysterectomy: Removal of the uterus, and sometimes the cervix, ovaries, and nearby lymph nodes.
- Trachelectomy: Removal of the cervix while leaving the uterus intact, often used for women who wish to preserve fertility.
-
Radiation Therapy.
- High-energy radiation is used to destroy cancer cells or shrink tumors, often used in combination with chemotherapy for advanced stages.
-
Chemotherapy.
- Chemotherapy drugs are used to kill cancer cells and shrink tumors, often in combination with radiation therapy.
-
Targeted Therapy.
- Targets specific molecules that drive cancer cell growth. This is often used in advanced or recurrent cervical cancer.
-
Immunotherapy.
- A newer treatment that helps the immune system recognize and attack cancer cells more effectively.
Women’s Health and Cervical Cancer.
Cervical cancer is a significant concern in women’s health. Regular screening and prevention strategies (like the HPV vaccine) are essential to protect women from this disease. Early detection is critical, as cervical cancer is one of the few cancers that can be prevented with proper screening and timely treatment of precancerous changes.
Cervical Cancer Awareness.
Raising awareness about cervical cancer is key to preventing it. Awareness campaigns help educate women about:
- The importance of regular screening (Pap smears and HPV tests).
- The role of the HPV vaccine in preventing infection by high-risk HPV strains.
- How early detection significantly increases the chances of successful treatment.
- The lifestyle choices (such as smoking cessation and safe sexual practices) that reduce the risk.
Promoting awareness encourages women to take preventive steps and seek medical attention promptly if they notice symptoms.
How to Prevent Cervical Cancer.
While cervical cancer can be caused by multiple factors, many prevention strategies focus on HPV, which is the leading cause:
-
HPV Vaccination.
- The HPV vaccine protects against the most common strains of the virus, especially types 16 and 18, which are responsible for most cervical cancers.
- It is recommended for both girls and boys between the ages of 9 and 14 and can be given up to age 45.
-
Regular Screening.
- Women aged 21–65 should get Pap smears and HPV tests according to recommended guidelines to detect abnormal cells before they become cancerous.
- Early detection through screening is crucial for preventing cervical cancer.
-
Practice Safe Sex.
- Use condoms to reduce the risk of HPV and other sexually transmitted infections.
- Limiting the number of sexual partners can also lower the chances of HPV exposure.
-
Quit Smoking.
- Smoking increases the risk of cervical cancer by weakening the immune system and making it harder to clear HPV infections.
-
Maintain a Healthy Immune System.
-
- A strong immune system helps prevent the persistence of HPV infections. Eating a healthy diet, exercising, and avoiding immunosuppressive conditions can all contribute to better immune health.
-
Also read about: 5 Yoga Poses to Relieve Menstrual Cramps.
Conclusion
Cervical cancer is largely preventable through vaccination, regular screening, and lifestyle changes. Awareness of the risk factors and early symptoms can help women seek timely medical intervention. By following preventive measures such as HPV vaccination, practicing safe sex, and maintaining regular check-ups, women can significantly reduce their risk of cervical cancer and ensure better health outcomes.
Resources:
[Link to a related article “How to Prevent Cervical Cancer”]