Learn the key differences and overlaps PCOS vs endometriosis. Explore symptoms, causes, diagnosis, treatment options, and practical tips for managing these common reproductive health conditions.
Introduction:
Polycystic Ovary Syndrome (PCOS) and endometriosis are two of the most common reproductive health conditions affecting women worldwide. Both can interfere with fertility, menstrual cycles, and overall well-being. Despite some overlapping symptoms, they are distinct disorders with different underlying causes, clinical manifestations, and treatment approaches. Misunderstanding the differences can delay diagnosis and treatment, making it crucial for women to understand the signs, symptoms, and management options for both conditions. This article provides a detailed guide to help women identify key differences, understand overlaps, and take proactive steps toward effective management.
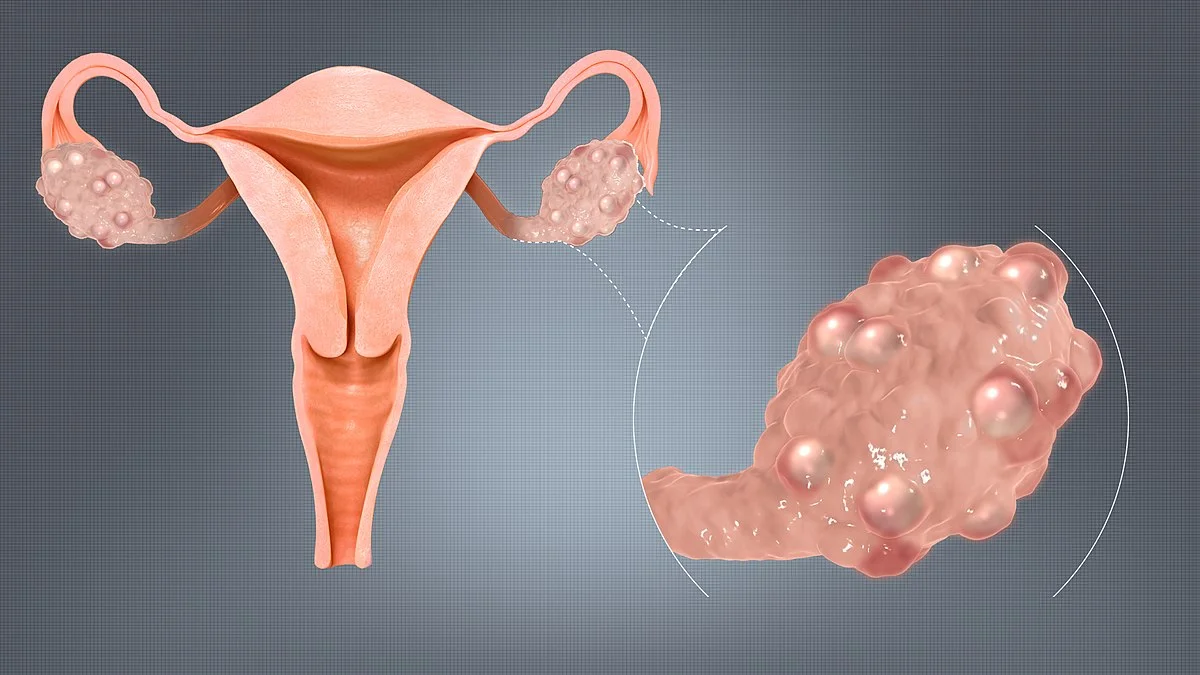
Understanding PCOS
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects approximately 5–10% of women of reproductive age. The condition is characterized by an imbalance in reproductive hormones, particularly androgens (male hormones), which can affect ovulation and menstrual cycles. Women with PCOS often experience a range of symptoms, including irregular periods, excessive hair growth, acne, and weight gain.
Causes of PCOS
The exact cause of PCOS is not fully understood, but several factors contribute to its development:
-
Hormonal imbalance: Elevated androgen levels disrupt ovulation.
-
Insulin resistance: Many women with PCOS have insulin resistance, increasing the risk of type 2 diabetes.
-
Genetic factors: PCOS can run in families, indicating a hereditary component.
-
Lifestyle influences: Diet, sedentary behaviour, and obesity can worsen symptoms.
Common Symptoms of PCOS
-
Irregular or missed menstrual periods
-
Excess facial or body hair (hirsutism)
-
Acne or oily skin
-
Thinning hair or hair loss on the scalp
-
Weight gain, especially around the abdomen
-
Darkened skin patches (acanthosis nigricans)
-
Difficulty conceiving due to irregular ovulation
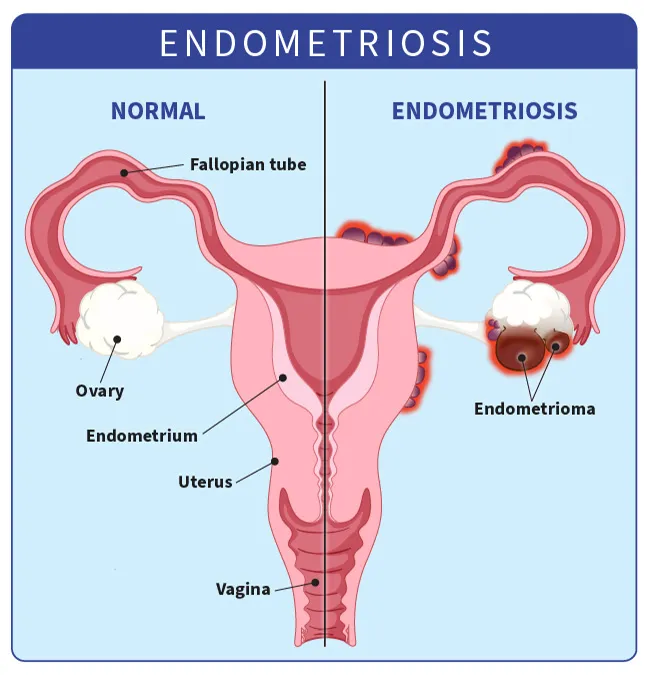
Understanding Endometriosis
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, often on the ovaries, fallopian tubes, or pelvic lining. Unlike PCOS, which is primarily hormonal, endometriosis involves inflammatory processes and can cause significant pain. It affects approximately 10% of women of reproductive age and is a leading cause of infertility.
Causes of Endometriosis
The exact cause of endometriosis remains unclear, but several theories exist:
-
Retrograde menstruation: Menstrual blood flows backward into the pelvic cavity.
-
Immune system dysfunction: The immune system may fail to eliminate endometrial tissue outside the uterus.
-
Genetic predisposition: Women with a family history are at higher risk.
-
Hormonal influence: Estrogen promotes growth of endometrial tissue.
Common Symptoms of Endometriosis
-
Painful periods (dysmenorrhea)
-
Pelvic pain between periods
-
Pain during intercourse (dyspareunia)
-
Heavy or irregular menstrual bleeding
-
Infertility or difficulty conceiving
-
Gastrointestinal symptoms such as bloating, diarrhea, or constipation
Key Differences Between PCOS vs Endometriosis
While PCOS and endometriosis share some overlapping features, the differences in cause, symptom patterns, and treatment are significant:
| Feature | PCOS | Endometriosis |
|---|---|---|
| Cause | Hormonal imbalance, genetics, insulin resistance | Endometrial tissue outside uterus, inflammation, immune dysfunction |
| Menstrual Pattern | Irregular, infrequent, or absent cycles | Usually regular cycles with severe pain |
| Pain | Mild pelvic discomfort; may experience cyst-related pain | Severe pelvic pain, especially during periods and intercourse |
| Fertility Impact | Ovulation disruption; irregular cycles affect conception | Physical blockage or adhesions affect conception |
| Other Symptoms | Excess hair growth, acne, weight gain | Gastrointestinal issues, chronic pelvic pain |
| Diagnosis | Blood tests, ultrasound | Ultrasound, MRI, laparoscopy (definitive) |
Overlapping Symptoms
Both PCOS and endometriosis can present with irregular periods, infertility, and pelvic discomfort, making diagnosis challenging. Women may also experience fatigue, mood swings, and difficulty maintaining hormonal balance. Because of these overlaps, a thorough medical evaluation is essential to distinguish between the two conditions and ensure proper treatment.
Diagnosis and Medical Evaluation
PCOS Diagnosis
A healthcare provider may diagnose PCOS based on:
-
Detailed medical history and physical examination
-
Blood tests to measure hormone levels, including androgens and insulin
-
Pelvic ultrasound to detect ovarian cysts
Endometriosis Diagnosis
Endometriosis diagnosis typically involves:
-
Pelvic examination to detect abnormalities
-
Ultrasound or MRI to visualize lesions (though small lesions may be missed)
-
Laparoscopy, a minimally invasive surgical procedure, which is considered the gold standard for definitive diagnosis
Treatment Options
PCOS Treatment
-
Lifestyle modifications: Healthy diet, regular exercise, and weight management
-
Medications: Hormonal treatments to regulate periods and reduce androgen levels
-
Fertility treatments: Ovulation induction or assisted reproductive technologies if conception is desired
Endometriosis Treatment
-
Pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs)
-
Hormonal therapy: Birth control pills, GnRH agonists, or progestins to reduce tissue growth
-
Surgery: Laparoscopic removal of lesions in severe cases
-
Fertility support: IVF or other reproductive treatments if conception is affected
Practical Tips for Managing Symptoms
-
Track menstrual cycles and symptoms to aid in diagnosis and management
-
Exercise regularly to improve hormonal balance and reduce discomfort
-
Consult a gynecologist for personalized treatment and follow-up
-
Consider support groups or counseling to manage emotional impact
FAQ
Q: Can a woman have both PCOS and endometriosis?
A: Yes, although rare, it is possible to have both conditions simultaneously. This can complicate symptoms and may require specialized treatment strategies.
Q: Are these conditions hereditary?
A: Both PCOS and endometriosis have genetic components. Women with a family history may have a higher risk, but environmental and lifestyle factors also play a role.
Q: How do I know which condition I have?
A: A combination of medical history, symptom tracking, hormone tests, and imaging studies helps doctors differentiate between PCOS and endometriosis. Laparoscopy can provide a definitive diagnosis for endometriosis.
Q: Can lifestyle changes help with these conditions?
A: Yes, diet, exercise, stress management, and weight control can improve symptoms and overall reproductive health, particularly for PCOS.
Q: Do these conditions affect fertility?
A: Both can impact fertility, but in different ways. PCOS affects ovulation, while endometriosis can cause structural changes or adhesions. Early diagnosis and treatment improve outcomes.
Conclusion
PCOS and endometriosis are distinct yet occasionally overlapping reproductive health conditions. Understanding their differences in causes, symptoms, and treatments is crucial for effective management and maintaining quality of life. Women experiencing irregular periods, pelvic pain, or difficulty conceiving should seek professional medical advice. Early diagnosis, proper treatment, and lifestyle adjustments can make a significant difference in managing both PCOS and endometriosis.